Introduction
Climate change, together with other natural and human-made health stressors, influences human health and disease in numerous ways. Some existing health threats will intensify and new health threats will emerge. Not everyone is equally at risk. Important considerations include age, economic resources, and location. Preventive and adaptive actions, such as setting up extreme weather early warning systems and improving water infrastructure, can reduce the severity of these impacts, but there are limits to the effectiveness of such actions in the face of some projected climate change threats.
Climate change presents a global public health problem, with serious health impacts predicted to manifest in varying ways in different parts of the world. Public health in the U.S. can be affected by disruptions of physical, biological, and ecological systems, including disturbances originating in the U.S. and elsewhere. Health effects of these disruptions include increased respiratory and cardiovascular disease, injuries and premature deaths related to extreme weather events, changes in the prevalence and geographical distribution of food- and waterborne illnesses and other infectious diseases, and threats to mental health.
boy sneezing
©Jose Luis Pelaez, Inc./Blend Images/Corbis
Key weather and climate drivers of health impacts include increasingly frequent, intense, and longer-lasting extreme heat, which worsens drought, wildfire, and air pollution risks; increasingly frequent extreme precipitation, intense storms, and changes in precipitation patterns that lead to drought and ecosystem changes (Ch. 2: Our Changing Climate); and rising sea levels that intensify coastal flooding and storm surge (Ch. 25: Coasts). Key drivers of vulnerability include the attributes of certain groups (age, socioeconomic status, race, current level of health – see Ch. 12: Indigenous Peoples for examples of health impacts on vulnerable populations) and of place (floodplains, coastal zones, and urban areas), as well as the resilience of critical public health infrastructure. Multi-stressor situations, such as impacts on vulnerable populations following natural disasters that also damage the social and physical infrastructure necessary for resilience and emergency response, are particularly important to consider when preparing for the impacts of climate change on human health.
Air Pollution
Climate change is projected to harm human health by increasing ground-level ozone and/or particulate matter air pollution in some locations. Ground-level ozone (a key component of smog) is associated with many health problems, such as diminished lung function, increased hospital admissions and emergency room visits for asthma, and increases in premature deaths.,,,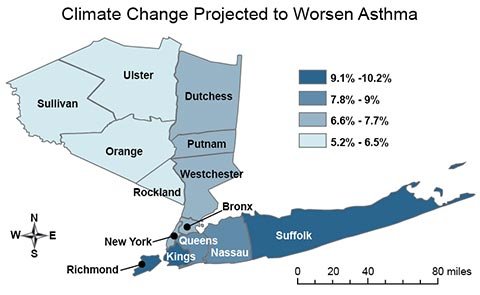
Figure 9.1: Climate Change Projected to Worsen Asthma
Climate Change Projected to Worsen Asthma
Details/Download
Factors that affect ozone formation include heat, concentrations of precursor chemicals, and methane emissions, while particulate matter concentrations are affected by wildfire emissions and air stagnation episodes, among other factors., By increasing these different factors, climate change is projected to lead to increased concentration of ozone and particulate matter in some regions.,,,,,,,,,
Increases in global temperatures could cause associated increases in premature deaths related to worsened ozone and particle pollution. Estimates made assuming no change in regulatory controls or population characteristics have ranged from 1,000 to 4,300 additional premature deaths nationally per year by 2050 from combined ozone and particle health effects.,, There is less certainty in the responses of airborne particles to climate change than there is about the response of ozone. Health-related costs of the current effects of ozone air pollution exceeding national standards have been estimated at $6.5 billion (in 2008 U.S. dollars) nationwide, based on a U.S. assessment of health impacts from ozone levels during 2000 to 2002.,
Allergens
Climate change, resulting in more frost-free days and warmer seasonal air temperatures, can contribute to shifts in flowering time and pollen initiation from allergenic plant species, and increased CO2 by itself can elevate production of plant-based allergens.,,,,,, Higher pollen concentrations and longer pollen seasons can increase allergic sensitizations and asthma episodes,,,, and diminish productive work and school days.,,
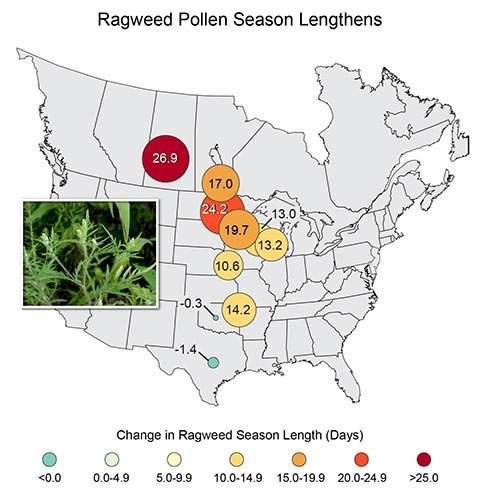
Figure 9.2: Ragweed Pollen Season Lengthens
Ragweed Pollen Season Lengthens
Details/Download
Simultaneous exposure to toxic air pollutants can worsen allergic responses.,,, Extreme rainfall and rising temperatures can also foster indoor air quality problems, including the growth of indoor fungi and molds, with increases in respiratory and asthma-related conditions.,,, Asthma prevalence (the percentage of people who have ever been diagnosed with asthma and still have asthma) increased nationwide from 7.3% in 2001 to 8.4% in 2010. Asthma visits in primary care settings, emergency room visits, and hospitalizations were all stable from 2001 to 2009, and asthma death rates per 1,000 persons with asthma declined from 2001 to 2009. To the extent that increased pollen exposures occur, patients and their physicians will face increased challenges in maintaining adequate asthma control.
Wildfires
Climate change is currently increasing the vulnerability of many forests to wildfire. Climate change is projected to increase the frequency of wildfire in certain regions of the United States (Ch. 7: Forests).,,,,, Long periods of record high temperatures are associated with droughts that contribute to dry conditions and drive wildfires in some areas. Wildfire smoke contains particulate matter, carbon monoxide, nitrogen oxides, and various volatile organic compounds (which are ozone precursors)and can significantly reduce air quality, both locally and in areas downwind of fires.,,,,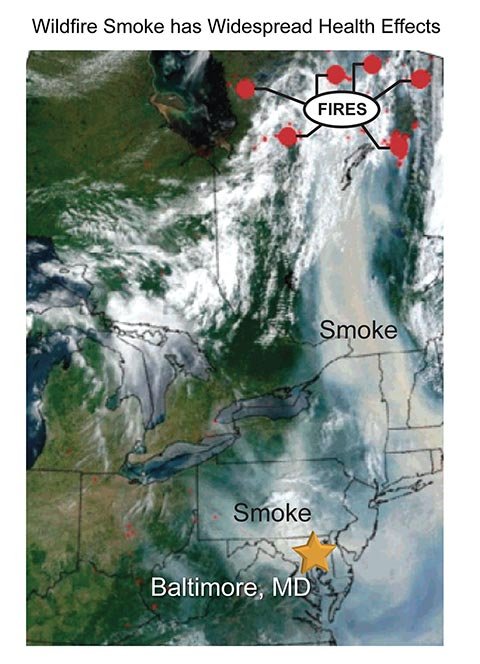
Figure 9.3: Wildfire Smoke has Widespread Health Effects
Wildfire Smoke has Widespread Health Effects
Details/Download
Smoke exposure increases respiratory and cardiovascular hospitalizations, emergency department visits, and medication dispensations for asthma, bronchitis, chest pain, chronic obstructive pulmonary disease (commonly known by its acronym, COPD), respiratory infections, and medical visits for lung illnesses.,, It has been associated with hundreds of thousands of deaths annually, in an assessment of the global health risks from landscape fire smoke.,,,, Future climate change is projected to increase wildfire risks and associated emissions, with harmful impacts on health.,,,,,,
Temperature Extremes
Extreme heat events have long threatened public health in the United States.,,, Many cities, including St. Louis, Philadelphia, Chicago, and Cincinnati, have suffered dramatic increases in death rates during heat waves. Deaths result from heat stroke and related conditions,,,,, but also from cardiovascular disease, respiratory disease, and cerebrovascular disease., Heat waves are also associated with increased hospital admissions for cardiovascular, kidney, and respiratory disorders.,,,, Extreme summer heat is increasing in the United States (Ch. 2: Our Changing Climate, Key Message 7), and climate projections indicate that extreme heat events will be more frequent and intense in coming decades (Ch. 2: Our Changing Climate, Key Message
Congratulations @punitha! You have completed some achievement on Steemit and have been rewarded with new badge(s) :
Click on any badge to view your own Board of Honor on SteemitBoard.
For more information about SteemitBoard, click here
If you no longer want to receive notifications, reply to this comment with the word
STOPHi! I am a robot. I just upvoted you! I found similar content that readers might be interested in:
http://nca2014.globalchange.gov/report/sectors/human-health