All we care about is whether we're breathing or not breathing, and adequately as well.
The act of breathing is autonomic, meaning you don't have to think about breathing. Your body just does it. However, there are some instances that can derail adequate breathing.

Brain trauma or a brain abscess are examples, but our focus today are diseases and insults to the lung that can make adequate breathing a difficult thing to accomplish, as those are more common.
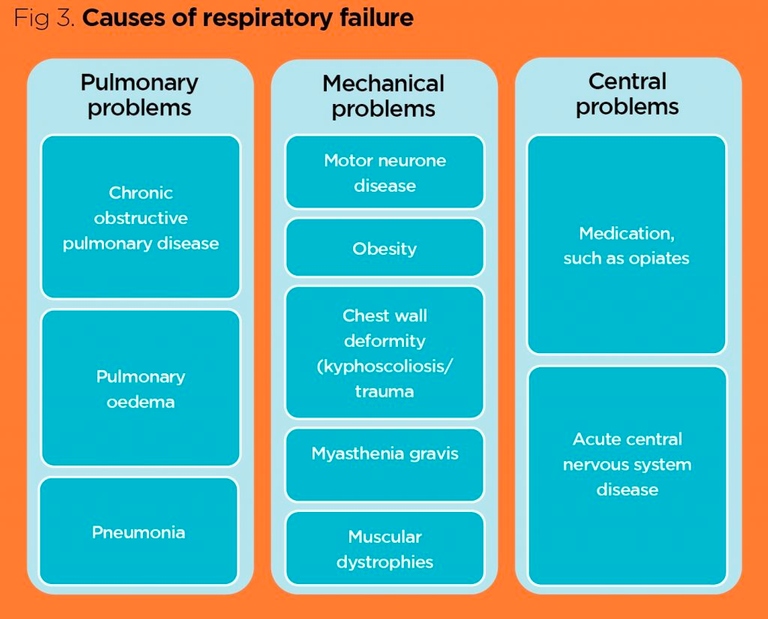
Let's start with discussing the most dangerous causes: Pulmonary Embolism and Respiratory Failure.
Acute Conditions
A pulmonary embolism can stop you from breathing, and shortness of breath can lead to respiratory failure.
Pulmonary embolisms typically occur in older adults that all of a sudden complain about difficultly breathing and coughing. Signs associated with it include:
- Pink-tinged frothy sputum
- Fast heart rate
- Pale skin
- A feeling of impending doom
What makes an older adult at risk for pulmonary embolisms?
- having atrial fibrillation
- undergoing estrogen therapy
- SMOKING
- cancer
- pregnancy
- long bone fractures
- prolonged inactivity, such as on long plane flights or car drives
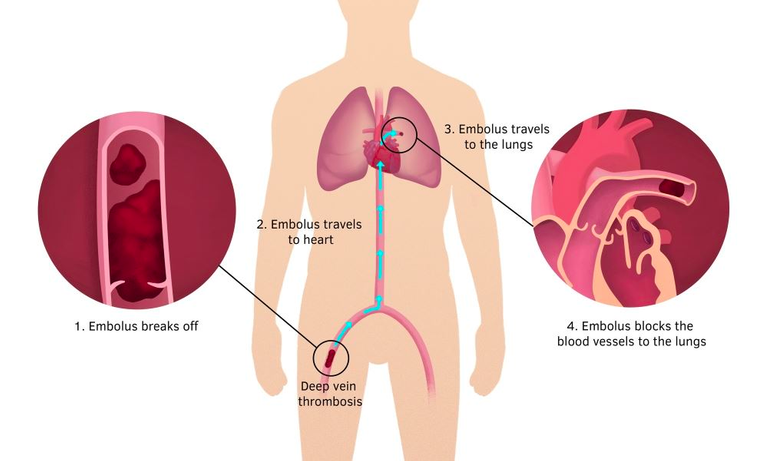
Obviously, pulmonary embolisms are life-threatening situations, so this is a trip straight to the emergency room, where medical staff will attempt to dissolve the clot with a blood thinning medication or surgically remove the clot.
Respiratory failure typically occurs in asthmatics, and they usually present with fast breathing, a fast heart rate (but sometimes slow), blue-tinged skin, and anxiety. You'll also notice an asthmatic using accessory muscles (rib muscles) to help support breathing and will have a difficult time forming complete sentences.
If onboard inhalers or nebulizer treatment fails, then treatment would be immediate injection of an epinephrine pen, a trip to the ER, and application of oxygen. In the ER, this person may be provided steroids, antihistamines, and an acid reducer.
Chronic Conditions
A person with a history of a condition that causes shortness of breath will get their lungs listened to. You have to note that the lungs are divided into upper lobes that produce bronchial/louder breath sounds and lower lobes that produce vesicular/soft/low breath sounds. Here are some of the typical sounds a doctor may hear or attempt to feel for:
Egophony
- Sounds like "eee", which is more pronounced in the upper lobes, and should NOT sound like "bahhh".
Tactile Fremitus
- When you say "99" or "1-2-3", vibrations will be stronger on the upper lobes vs the lower lobes, and should NOT be reversed.
Whispered Pectoriloquy
- Just like tactile fremitus, but whispered. Whisper should NOT be heard on the lower lobes.
Percussion
- This is where they will use their fingers to tap on your back like a hammer. What they are listening for is resonance. If there is hyperresonance/tympany, then this could indicate chronic obstructive pulmonary disease. However, if dull, then this could indicate consolidation/pleural effusion, which is a sign of bacterial pneumonia.
The doctor or provider then may perform what is called a pulmonary function test, also known as a PFT. It can measure the severity of OBSTRUCTIVE or RESTRICTIVE pulmonary dysfunction.
The categorizations of obstructive include diseases, such as asthma, COPD, and bronchiectasis. Restrictive pulmonary dysfunction include diseases, such as pulmonary fibrosis, pleural disease, and obstruction of the diaphragm.
Most commonly, the doctor or provider will see obstructive lung diseases in office. These include:
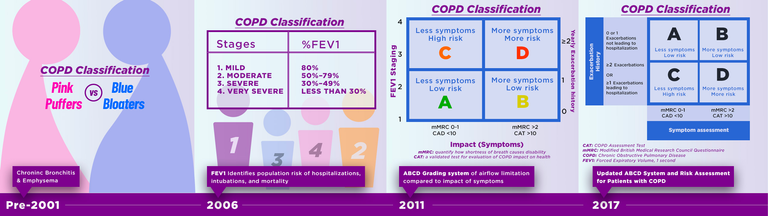
Chronic Obstructive Pulmonary Disease (COPD)
- Includes emphysema and chronic bronchitis
- loss of elasticity of the lungs
- smoking and older age are risk factors
Chronic Bronchitis
- Diagnosed if coughing with mucoid productive has been going on for at least 3 months of the year for at least 2 consecutive years.
Emphysema
- Chronic hyperinflation of the lungs with prolonged expiration.
- Risk factors include smoking, older age, exposure to coal, and deficiency of Alpha-1 trypsin.
When it comes to treatment:
COPD is treated based off its categorization developed by the Global Initiative for Chronic Obstructive Lung Disease (GOLD):
- Category A - low risk of exacerbation, use of short active beta-2 agonist (SABA), such as albuterol, alone or in combination with a short-acting anticholinergic inhaler, such as Atrovent.
- Category B - low risk of exacerbation, and treated with a long-acting B2 agonist (LABA), such as Salmeterol or formoterol. Long-acting anticholinergics aka long-acting muscarinic agents (LAMA), such as Tiotropium (Spiriva) or Ellipta can also be used instead.
- Category C - high risk of exacerbation, and treated with LAMA as the first choice, but then switch to combo LAMA-LABA if uncontrolled, or continue with LAMA and add theophylline.
- Category D - high risk of exacerbation, in which you would be referred to a pulmonologist.
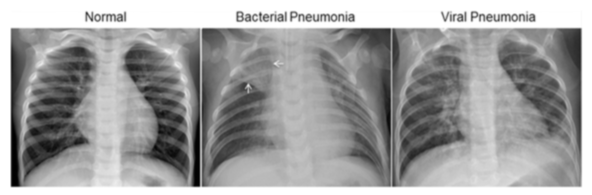
COPD also puts the patient at risk for bacterial pneumonia, in where the patient would present with a high fever, green sputum, and worsened wheezing and shortness of breath. Typically, the patient would get an x-ray to check for consolidation or pooling of fluid in the lungs. If found, the patient will then receive a prescription of antibiotics, such as Bactrim DS, doxycycline, ceftin, augmentin, and sometimes steroids to calm the inflammation.
Community-Acquired Bacterial Pneumonia (CAP)
- Acute bacterial pneumonia (CAP) - acute onset, high fever, chills, productive cough, green sputum, and pleuritic chest pain
- Strep penumoniae - crackles, dull breath sounds, elevated leukocytes and neutorphils
- Atypical/Walking Pneumonia - gradual, low grade fever, headache, sore throat, cough, wheezing, interstitial infiltrates on chest xray
- Viral Pneumonia - fever, cough, pleurisy, SOB, muscle aches, decreased breath sounds
- Acute Bronchitis - dry and severe cough that wakes you up at night, light colored sputum, can last 4-6 weeks, and antibiotics aren't necessary
Pneumonia criteria for hospital admission:
- Age 60 or older with acute mental change and congestive heart failure
- multiple lobar involvement
- alcoholic
- CURB-65 presentation: confusion, urea > 19.6 mg/dL, respiration > 30 bpm, blood pressure < 90/60 mmHg
Atypical Pneumonia aka Walking Pneumonia
- More common in children and young adults, and very contagious
- Wheezing and diffused crackles/rales
- Clear mucus
- Diffused interstitial infiltrates on chest x-ray
- Treated with macrolides, such as doxycycline, antitussives, and hydration
Acute Bronchitis
- Typically viral, but sometimes bacterial infection of the bronchi, which causes inflammation in the lungs, resulting in increased reactivity of the upper airways.
- Viral causes include adenoviruses, influenza, coronaviruses, RSV, to name a few.
- Presents with wheezing, rhonchi, resonance, a NORMAL chest x-ray, and may have no fever to a low-grade fever
- No antibiotics are administered as this is viral, but instead the patient should increase hydration, stop smoking, and can take dextromethorphan (found over-the-counter, such as Robitussin) or Tessalon Perles. Can inhale albuterol if short of breath. Short term steroids if the patient has severe wheezing.
Pertussis aka Whooping Cough
- Caused by a gram negative bacteria called Bordetella pertussis
- At least 14 days of paroxysmal coughing, inspiratory whooping, low grade fever, runny nose
- 3 stages: catarrhal - infectious period, paroxysmal, and convalescent stage
- elevated white blood cells, lymphocytosis (80% lymphocytes in WBC differential), and the chest x-ray should be negative
- Macrolides, such as Azithromycin or Erythomycin, to treat.
Cold
- viral infection lasting 4-10 days, with the most contagious period at 2-3 days. Transmitted by respiratory droplets.
- presents with sometimes fever, sore throat, but has frequent sneezing, nasal congestion, watery eyes, and runny nose.
- treat with hydration, rest, hand washing, over-the-counter analgesics, decongestants, antitussives, and antihistamines.
Tuberculosis
- bacterial infection, caused by Mycobacterium tuberculosis, that can infect mostly the lungs, but also the kidneys, brain, lymph, adrenals, and bone.
- a chest x-ray will demonstrate granulomas in the lungs
- typically seen in high-risk regions where TB is endemic, migrant workers, drug users, homeless, inmates, nursing homes, and amongst the immunocompromised population.
- active vs latent, where latent is not infectious, but would still need treatment
- initial detection with a Mantoux skin test, but may have a false-positive reaction if the person received the BCG Vaccination. If false-positive is suspected, the a Quantiferon Gold blood draw is indicated.
- Drugs used for treatment include INH, rifampin, ethambutol and pyrazinamide, taken three times a week - duration is based on compliance for taking medication
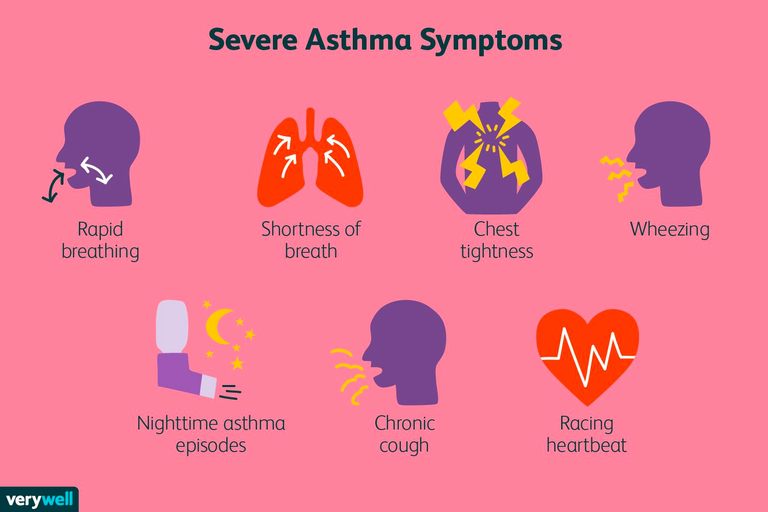
Asthma
- reversible airway obstruction
- genetically linked with a family history of allergies, eczema, and allergic rhinitis
- life-threatening is known as status asthmaticus
- presents with wheezing with a prolonged expiratory phase and rapid heart rate
- treatment includes inhalers, nebulizer treatment, a short course of oral corticosteroids
- "Rescue" inhalers include short acting beta 2 agonists, such as albuterol
- "Maintenance" or long term control of asthma includes inhaled corticosteroids (ICS) by itself or in combination with a LABA.
- Never use LABA's as monotherapy, as it can increase the risk of death from asthma.
As review of of the different drug classes:
Inhaled corticosteroids (ICS) - Triamcinolone (Azmacort), Budesonide (Pulmicort), Fluticasone (Flovent).
Long Acting Beta Agonist (LABA) - Salmeterol (Serevent), Formoterol (Foradil)
Combo ICS-LABA - Salmeterol+Fluticasone (Advair), Budesonide+Formoterol (Symbicort)
Other adjust asthma treatment includes leukotriene inhibitors, such as montelukast, and mast cell stabilizers, such as cromolyn, and methylxanthines, such as theophylline.
Just like COPD, Asthma also has it's own classification, and depending on the severity will determine how aggressive the treatment is:
- Step 1 - Intermittent asthma (FEV1>80% predicted with Spirometry) - use SABA, such as albuterol inhaler
- Step 2 - Mild persistent asthma (FEV1>80% predicted with Spirometry) - use SABA, and add a low-dose inhaled corticosteroid, such as Flovent or QVAR. Can add a leukotriene inhibitor, such as montelukast.
- Step 3 - Moderate persistent asthma (FEV1 60-80% predicted with Spirometry) - use SABA, and add either a low-dose ICS-LABA combo or a medium-dose ICS.
- Step 4 - Severe persistent asthma (FEV1<60% predicted with Spirometry) - use SABA as needed, but add a medium-dose ICS-LABA combo.
Quick note: There is also such thing as Exercised-Induced Asthma or Bronchospasm, and it is recommended to inhale a SABA, such as albuterol, 15 minutes prior to exercising.
Also another note: Long term use of high-dose inhaled steroids can lead to osteoporosis, slow growth in children, glaucoma, cataracts, immune suppression, hypothalamic-pituitary-adrenal suppression, just as if any person taking high dose steroids in any form.
Phew, I know that was exhaustive and a lot to absorb, but everything I mentioned are the most common things you'll see when it comes to the lungs. Obviously, the topic can go into so much more detail, but you should refer to medical books for that. Everything here was really just the tip of the iceberg, and I hope that in review, you're able to recognize some of the aforementioned and what the treatment options are.
Comment down below if you're curious about what a particular lung condition not listed above. Stay healthy, and exercise those lungs!
Congratulations @nine-minute! You have completed the following achievement on the Hive blockchain and have been rewarded with new badge(s):
Your next payout target is 50 HP.
The unit is Hive Power equivalent because your rewards can be split into HP and HBD
You can view your badges on your board and compare yourself to others in the Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPTo support your work, I also upvoted your post!
Check out the last post from @hivebuzz:
Support the HiveBuzz project. Vote for our proposal!