Most people are familiar with the pay-for-service model in healthcare.
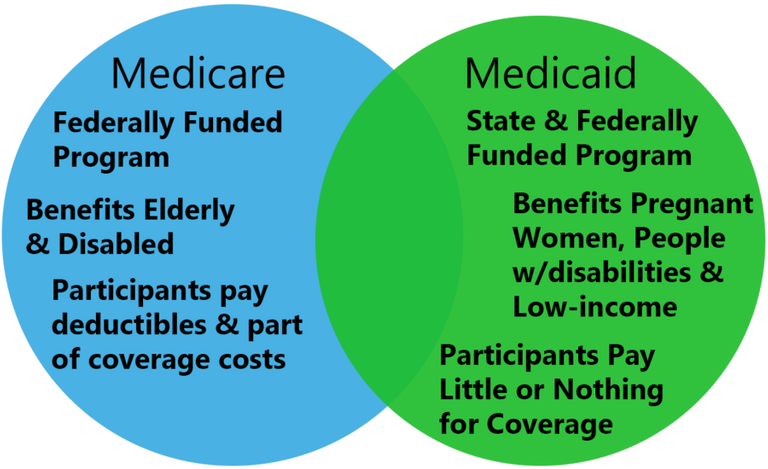
That was long long time ago. Today, medical coverage is mainly provided by insurers, and in the United States, the major players are Medicare and Medicaid. The picture below differentiates between the two:
Your physician provides you a service, but doesn't outright drop a $10k bill on you. Instead, he or she bills your insurance that you pay for monthly.
However, let's dive a little deeper into the nuances of the history of billing, where it stands today, and how does it differ between medical doctors and nurse practitioners.
Back in 1965, there were really only physicians. Nurse Practitioners didn't exist then, so all the rules that exist today that govern Medicare and Medicaid were covered by a now out-dated Social Security Act.
The Social Security Act allows for physicians to bill Medicare and Medicaid for their direct care of patients in the hospital, hospices, nursing homes, etc... you get the picture.
Problem is now... the Social Security Act hasn't been updated to include nurse practitioners... at least not to a full extent. This has led to a lot of confusion for billing as the nurse practitioner role evolves. There has been some progress though!
In 1997, the Budget Reconciliation Act removed a statute that restricted reimbursement for services performed by a nurse practitioner. Now, NP's can get reimbursed for 80-85% for the same services rendered by a physician.
However, there are ways to get reimbursed more - that is if an NP works at a medical practice with a physician, and the physician shares the visit with the NP.
Obviously, the above scenario can make billing fraud from NP's a possibility, and regulatory bodies and insurers are always looking for potential fraud and abuse of billing. That is why audits of hospitals, clinics, and places where healthcare services are provided exist.

Billing fraud isn't the only thing that CMS is on the look out for.
The Stark Act states that a physician cannot refer a patient to an immediate family member or another office where that physician can attain financial gain. However, the Stark Act doesn't mention NP's, but it is implied that NP's can still violate the Stark Act if the supervising physician urged them to refer for financial gain.
The Anti-Kickback Statute is a federal law that can criminally punish those that pay providers to refer patients to them.
Then there's specific requirements for providers when documenting, in order to appropriately bill Medicare and Medicaid.
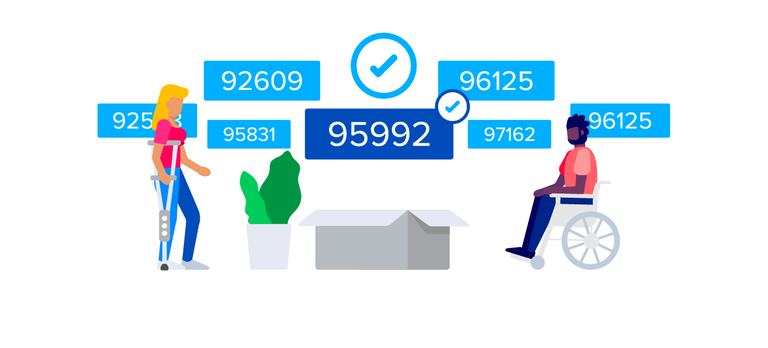
When insurers reimburse for patient services, they want to make sure that the billed services are consistent with what was found and treated for at the visit. Insurers do not want to get cheated out of their reimbursement, so oftentimes they will require to confirm appropriate documentation, before they approve covering for things like pain medication or an MRI.
Therefore, sets of rules were created for documentation, so they can be checked for appropriateness:
- Problem Focused — limited examination
- Expanded Problem Focused — limited examination and any other area
- Detailed — extended examination and any other area
- Comprehensive — general multisystem examination
These are all the things that a provider must abide to in order to practice. Not hard to remember them at all, am I right?
Hope this provides some insight on the things providers have to deal with outside of patient care, and also insight into how this may affect YOUR care.
That sound a bit complicated. But does the health care cost so much there in USA?
Very good question. I even wondered about that myself. According to this TIME's article, basically there is a shortage of doctors, so when you have a low supply of doctors and a high demand for them, the doctors become very very expensive. This extends to hospitals as well. It's also the case that our culture promotes that healthcare is a privilege, rather than a right to have. [Source]