Food-borne illness:
Food-borne illness (colloquially referred to as food poisoning, food-borne decease) is any illness resulting from the food spoilage of contaminated food, pathogenic bacteria, viruses, or parasites that contaminate food, as well as toxins such as poisonous mushrooms and various species of beans that have not been boiled for at least 10 minutes.
Symptoms:
Symptoms often include vomiting, fever, and aches, and may include diarrhea. Bouts of vomiting can be repeated with an extended delay in between because even in the infected food was eliminated from the stomach in the first bout, microbes (if applicable) can pass through the stomach into the intestine and begin to multiply. Some types of microbes stay in the intestine, some produce a toxin that is absorbed into the bloodstream, and some can directly invade deeper body tissues.
Causes:
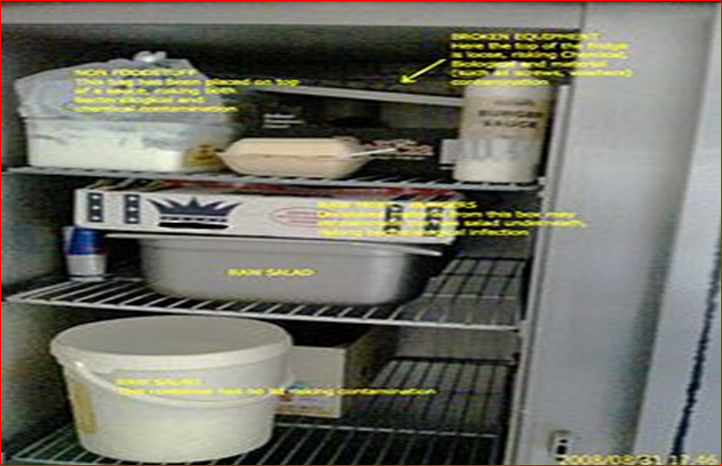
The Food-borne illness usually arises from improper handling, preparation, or food storage. Good hygiene practices before, during, and after food preparation can reduce the chances of contracting an illness.
Bacteria:
Bacteria are a common cause of food-borne illness. In the United Kingdom during 2000, the individual bacteria involved were the following: Campylobacter jejuni 77.3%, Salmonella 20.9%, Escherichia coli O157: H7 1.4%, and all others less than 0.56%. common bacterial food-borne pathogens are:
Campylobacter jejuni which can lead to secondary Guillain–Barré syndrome and periodontitis.
Clostridium perfringens, the "cafeteria germ".
Salmonella spp. – its S. typhimurium infection is caused by consumption of eggs or poultry that are not adequately cooked or by other interactive human-animal pathogens.
Escherichia coli O157:H7 enterohemorrhagic (EHEC) which can cause hemolytic-uremic syndrome
Enterotoxins:
In addition to disease caused by direct bacterial infection, some food-borne illnesses are caused by enterotoxins (exotoxins targeting the intestines). Enterotoxins can produce illness even when the microbes that produced them have been killed. Symptom appearance varies with the toxin but may be rapid in onset, as in the case of enterotoxins of Staphylococcus aureus in which symptoms appear in one to six hours.
Emerging food-borne pathogens:
Many food-borne illnesses remain poorly understood.
Aeromonas hydrophila, Aeromonas caviae, Aeromonas sobria
Preventing bacterial food poisoning:
Prevention is mainly the role of the state, through the definition of strict rules of hygiene and a public services of veterinary surveying of animal products in the food chain, from farming to the transformation industry and delivery (shops and restaurants). This regulation includes:
traceability: in a final product, it must be possible to know the origin of the ingredients (originating farm, identification of the harvesting or of the animal) and where and when it was processed; the origin of the illness can thus be tracked and solved (and possibly penalized), and the final products can be removed from the sale if a problem is detected;
enforcement of hygiene procedures such as HACCP and the "cold chain";
power of control and of law enforcement of veterinarians.
In August 2006, the United States Food and Drug Administration approved Phage therapy which involves spraying meat with viruses that infect bacteria, and thus preventing infection. This has raised concerns, because without mandatory labelling consumers would not be aware that meat and poultry products have been treated with the spray.
Mycotoxins and alimentary mycotoxicoses:
The term alimentary mycotoxicoses refers to the effect of poisoning by Mycotoxins (The term 'mycotoxin' is usually reserved for the toxic chemical products produced by fungi that readily colonize crops) through food consumption. Mycotoxins sometimes have important effects on human and animal health. For example, an outbreak which occurred in the UK in 1960 caused the death of 100,000 turkeys which had consumed aflatoxin-contaminated peanut meal. In the USSR in World War II, 5,000 people died due to Alimentary Toxic Aleukia (ALA). The common food-borne Mycotoxins include:
Aflatoxins – originated from Aspergillus parasiticus and Aspergillus flavus. They are frequently found in tree nuts, peanuts, maize, sorghum and other oilseeds, including corn and cottonseeds. The pronounced forms of Aflatoxins are those of B1, B2, G1, and G2, amongst which Aflatoxin B1 predominantly targets the liver, which will result in necrosis, cirrhosis, and carcinoma.[18][19] In the US, the acceptable level of total aflatoxins in foods is less than 20 μg/kg, except for Aflatoxin M1 in milk, which should be less than 0.5 μg/kg.
Altertoxins: are those of Alternariol (AOH), Alternariol methyl ether (AME), Altenuene (ALT), Altertoxin-1 (ATX-1), Tenuazonic acid (TeA) and Radicinin (RAD), originated from Alternaria spp. Some of the toxins can be present in sorghum, ragi, wheat and tomatoes.[23][24][25] Some research has shown that the toxins can be easily cross-contaminated between grain commodities, suggesting that manufacturing and storage of grain commodities is a critical practice.[26]
Citrinin
Citreoviridin
Cyclopiazonic acid
Cytochalasins
Ergot alkaloids / Ergopeptine alkaloids – Ergotamine
Fumonisins – Crop corn can be easily contaminated by the fungi Fusarium moniliforme, and its Fumonisin B1 will cause Leukoencephalomalacia (LEM) in horses, Pulmonary edema syndrome (PES) in pigs, liver cancer in rats and Esophageal cancer in humans. For human and animal health, both the FDA and the EC have regulated the content levels of toxins in food and animal feed.
• Fusaric acid
• Fusarochromanone
• Kojic acid
• Lolitrem alkaloids
• Moniliformin
• 3-Nitropropionic acid
• Nivalenol
• Ochratoxins – In Australia, The Limit of Reporting (LOR) level for Ochratoxin A (OTA) analyses in 20th Australian Total Diet Survey was 1 µg/kg,[31] whereas the EC restricts the content of OTA to 5 µg/kg in cereal commodities, 3 µg/kg in processed products and 10 µg/kg in dried vine fruits.
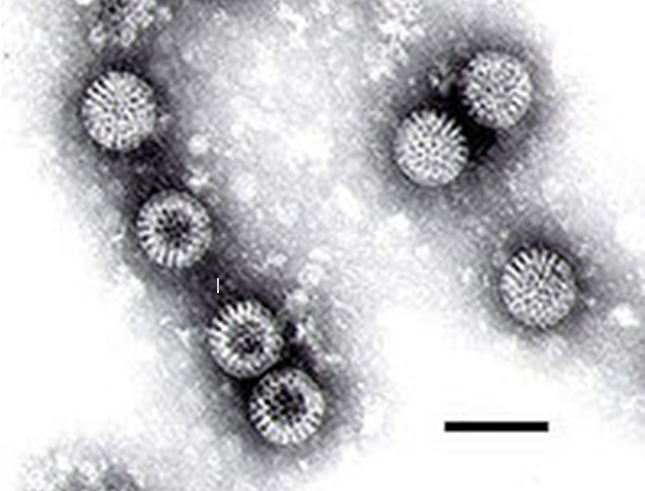
Viruses:
Viral infections make up perhaps one third of cases of food poisoning in developed countries. In the US, more than 50% of cases are viral and noroviruses are the most common food-borne illness, causing 57% of outbreaks in 2004. Food-borne viral infection are usually of intermediate (1–3 days) incubation period, causing illnesses which are self-limited in otherwise healthy individuals; they are similar to the bacterial forms described above.
• Enterovirus
• Hepatitis A is distinguished from other viral causes by its prolonged (2–6 week) incubation period and its ability to spread beyond the stomach and intestines into the liver. It often results in jaundice, or yellowing of the skin, but rarely leads to chronic liver dysfunction. The virus has been found to cause infection due to the consumption of fresh-cut produce which has fecal contamination.
• Hepatitis E
• Norovirus
• Rotavirus
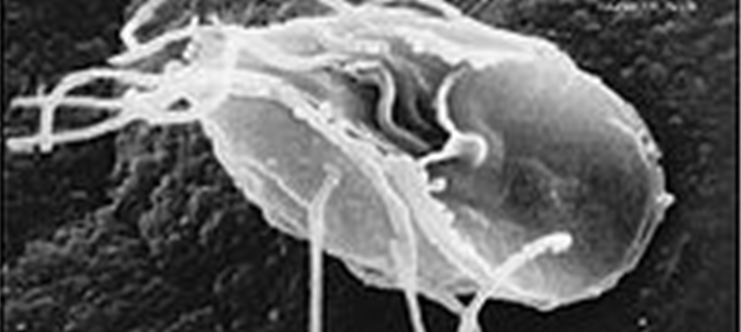
Parasites:
Most food-borne parasites are zoonoses.
Platyhelminthes:
Nematode
Protozoa
Giardia lamblia
Sarcocystis hominis
Sarcocystis suihominis
Toxoplasma gondiiHello Steemit Family! I hope all the family members will be fine and happy. I am @steemitwarker here with a very interesting and informative post... Today we'll talk about the Food-borne illness. So, first of all I consider it proper to explain on you what is food-borne illness...
Natural toxins:
Several foods can naturally contain toxins, many of which are not produced by bacteria. Plants in particular may be toxic; animals which are naturally poisonous to eat are rare. In evolutionary terms, animals can escape being eaten by fleeing; plants can use only passive defenses such as poisons and distasteful substances, for example capsaicin in chili peppers and pungent sulfur compounds in garlic and onions. Most animal poisons are not synthesised by the animal, but acquired by eating poisonous plants to which the animal is immune, or by bacterial action.
• Alkaloids
• Ciguatera poisoning
• Grayanotoxin (honey intoxication)
• Mushroom toxins
• Phytohaemagglutinin (red kidney bean poisoning; destroyed by boiling)
• Pyrrolizidine alkaloids
• Shellfish toxin, including paralytic shellfish poisoning, diarrhetic shellfish poisoning, neurotoxic shellfish poisoning, amnesic shellfish poisoning and ciguatera fish poisoning
• Scombrotoxin
• Tetrodotoxin (fugu fish poisoning)
Some plants contain substances which are toxic in large doses, but have therapeutic properties in appropriate dosages.
• Foxglove contains cardiac glycosides.
• Poisonous hemlock (conium) has medicinal uses.
Other pathogenic agents:
Other pathogenic agents are given below:
"Ptomaine poisoning"
In 1883, the Italian, Professor Salmi, of Bologna, introduced the generic name ptomaine (from Greek ptōma, "fall, fallen body, corpse") for alkaloids found in decaying animal and vegetable matter, especially (as reflected in their names) putrescine and cadaverine.
Mechanism:
Incubation period:
The delay between consumption of a contaminated food and appearance of the first symptoms of illness is called the incubation period. This ranges from hours to days (and rarely months or even years, such as in the case of listeriosis or bovine spongiform encephalopathy), depending on the agent, and on how much was consumed. If symptoms occur within one to six hours after eating the food, it suggests that it is caused by a bacterial toxin or a chemical rather than live bacteria.
The long incubation period of many food-borne illnesses tends to cause sufferers to attribute their symptoms to gastroenteritis.During the incubation period, microbes pass through the stomach into the intestine, attach to the cells lining the intestinal walls, and begin to multiply there.
Infectious dose:
The infectious dose is the amount of agent that must be consumed to give rise to symptoms of food-borne illness, and varies according to the agent and the consumer's age and overall health. Pathogens vary in minimum infectious dose; for example, Shigella sonnei has a low estimated minimum dose of < 500 colony-forming units (CFU) while Staphylococcus aureus has a relatively high estimate.In the case of Salmonella a relatively large inoculum of 1 million to 1 billion organisms is necessary to produce symptoms in healthy human volunteers, as Salmonellae are very sensitive to acid. An unusually high stomach pH level (low acidity) greatly reduces the number of bacteria required to cause symptoms by a factor of between 10 and 100.
Steemit:

Adsactly:

SEI(Steemit Education Initiative):

So Guys! I hope you'll like my post. Please don't forget to upvote my post.
Good bye till the next post...
source: wikipedia
https://en.wikipedia.org/wiki/Foodborne_illness
https://en.wikipedia.org/wiki/Foodborne_illness



Hi! I am a robot. I just upvoted you! I found similar content that readers might be interested in:
https://en.wikipedia.org/wiki/Foodborne_illness