Heart Disease: Causes of a Heart Attack What Is Heart Disease?
Heart disease refers to conditions that involve the heart, its vessels, muscles, valves, or internal electric pathways responsible for muscula )r contraction. Common heart disease conditions include:
)r contraction. Common heart disease conditions include:
Coronary artery disease
Heart failure
Cardiomyopathy
Heart valve disease
Arrhythmias
2 of 29
What Is a Heart Attack?
When a coronary artery becomes blocked (usually by a blood clot), an area of heart tissue loses its blood supply. This reduction of blood can quickly damage and/or kill heart tissue, so quick treatments in an emergency department and/or catheterization suite are necessary to reduce the loss of heart tissue. Loss of heart tissue due to a blockage can cause symptoms such as chest pain, shortness of breath, weakness, and even death. Quick treatments have reduced the number of deaths from heart attacks in recent years; however, about 610,000 people die from heart disease in the US each year (1 in every 4 deaths) according to the CDC.
3 of 29
Heart Attack Symptoms
The following are warning signs of a heart attack:
Chest pain (may spread to the back, neck, arms and/or jaw)
Dizziness
Nausea, vomiting
Rapid or irregular heartbeats
Shortness of breath
Some people may exhibit anxiety, indigestion and/or heartburn (some women may present with these as their predominant symptoms instead of chest pain)
Weakness
4 of 29
Heart Attack Symptoms in Women
Although some women present with symptoms of chest pain, a large number of women will not present with chest pain. Instead, women commonly have a different set of heart attack symptoms.
Know These Heart Attack Symptoms
Arrhythmias
Cough
Heartburn
Loss of appetite
Malaise
Such symptoms in women cause delays in diagnosis if the symptoms are not considered as possible signs of heart disease. Delays in diagnosis can cause further damage to heart tissue or even death.
5 of 29
Coronary Artery Disease Symptoms
Coronary artery disease (CAD) occurs when plaque, a sticky substance, narrows or partially block coronary arteries (like sticky material stopping up a straw) and can result in reduced blood flow. This minimise blood flow may cause chest pain (angina), a warning sign of potential heart problems such as a heart attack. Plaque may also trap small blood clots, complete obstructing a coronary artery suddenly, resulting in a heart attack.
6 of 29
How Plaque, Blood Clots can Cause Heart Attack
Plaque can occur in coronary and other arteries (for example, carotid arteries). Some plaque may be hard or firm on the outside, but soft and mushy or sticky on the inside. If the hard shell-like area cracks open, blood components like platelets and small blood clots form a large clot and effectively block blood flow through the artery. The heart tissue downstream from the clot then suffers from lack of blood and becomes damaged or dies.
7 of 29
Heart Attack Symptoms? Call 9-1-1
If you or an individual develop symptoms of a heart attack, do not delay getting medical help. Call 911 or have someone call for you. Do not drive yourself or others to a hospital as 911 emergency medical services (EMS) personnel can begin basic treatment immediately. Delaying care can result in increased heart damage or death.
8 of 29
Sudden Cardiac Arrest
A heart attack can cause other abnormalities besides blocking blood flow. For example, sudden cardiac death may occur when the heart’s electrical signals become erratic (arrhythmias). When the heart tissue that is responsible for regular electrical stimulus of heart muscle contractions is damaged, the heart stops effectively pumping blood. Death usually occurs in a few minutes after the heart stops pumping blood. Consequently, rapid coronary pulmonary resuscitation (CPR) and a restoration of the organized electrical activity (usually done by electric shock with a defibrillator) may restore effective pumping of blood. This can be lifesaving for some individuals.
9 of 29
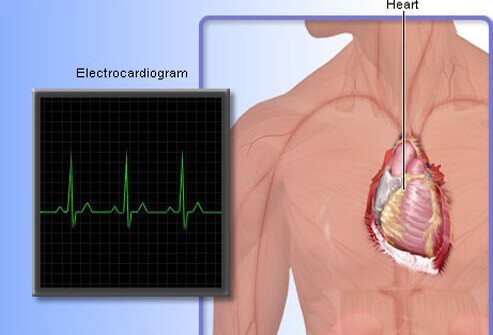
Erratic Heart Beat (Arrhythmia)
Patients who notice that their heartbeats are abnormally fast, slow, or irregular may be experiencing irregular electrical impulses termed arrhythmias. They may also have symptoms of weakness, shortness of breath, and anxiety. Arrhythmias can alter, slow or even stop the heart’s ability to pump blood. Consequently, individuals with arrhythmias should seek emergency medical care especially if the arrhythmia is persistent or causes any symptoms related to heart attack symptoms such as chest pain.
10 of 29
Cardiomyopathy
Cardiomyopathy is a condition indicated by abnormal heart muscle. Abnormal muscles make it harder for your heart to pump blood to the rest of the body.
Main Types of Cardiomyopathy
Dilated (stretched and thinned muscle)
Hypertrophic (thickened heart muscle)
Restrictive (rare problem where the heart muscle does not stretch normally so the chambers do not fill with blood properly)
Signs and Symptoms of Cardiomyopathy
Shortness of breath
Fatigue
Swelling of the feet, ankles and/or legs
Coughing when lying down
Dizziness
Chest pain
Irregular heartbeats
11 of 29
Heart Failure
Heart failure (also termed congestive heart failure) means the pumping action of the heart cannot meet the body’s demand for blood; it does not mean that the heart fails to pump - it does mean a failure in an aspect of the heart’s ability to complete an otherwise normal function. The symptoms and signs are almost identical to those seen with cardiomyopathy.
12 of 29
Congenital Heart Defect
A congenital heart defect is a defect in the development of the heart as an organ that is usually first noticed at birth although some are not found until adulthood. There are many types of congenital heart defects and a few need no treatment, but others may need surgical repair. The American Heart Association lists at least 18 distinct types of congenital heart defects - many of them have additional anatomical variations.
Congenital heart defects put those patients at higher risk to develop arrhythmias, heart failure, heart valve infections, and other problems. A cardiologist (often a pediatric cardiologist) needs to be consulted on how to treat these defects. Recent advances have allowed surgeons to repair many of these defects so that the patient can go on to develop normally.
13 of 29
Heart Disease Testing: EKG (Electrocardiogram)
The heart's electrical activity can be seen with an EKG (also termed ECG or electrocardiogram). EKGs are tests that provide important information to the physician about the heart rhythm, damage to the heart, or a heart attack, and may provide several other important pieces of information or clues to the patient's condition. In addition, EKGs can be compared to past and future EKGs to see changes in the heart’s electrical activity over time or after treatments.
14 of 29
Heart Disease Testing: Stress Test
A stress test measures the ability of a person's heart to respond to the body's demand for more blood during stress (exercise or work). A continual measurement of the heart's electrical activity (a continual EKG or rhythm strip) is recorded along with the heart rate and blood pressure as a person's stress (exercise) is gradually increased on a treadmill. The information helps to show how well the heart responds to the body's demands and may provide information to help diagnose and treat problems. It can also be used to see the effects of treatment on the heart.
15 of 29
Heart Disease Testing: Holter Monitor
Many people have intermittent symptoms such as intermittent chest pain or occasional feelings of their heart beating faster or irregularly. However, their EKG does not show any changes. To detect these intermittent changes, a device called a Holter monitor can be worn for several days to record the hearts’ electrical function.
A Holter monitor is similar to a stress test, but it is worn for 1 or 2 days and provides a continual EKG-like recording of the heart's electrical activity during those days. Most doctors will ask the patient to keep a logbook of the time they do certain activities (for example, walking a mile starting at 7:20 AM and ending at 7:40 AM) and list any symptoms (for example, "experienced shortness of breath or rapid irregular heartbeats at 7:35 AM"). The Holter monitor's recordings can then be examined based on when certain symptoms occurred.
16 of 29
Heart Disease Testing: Chest X-ray
Chest x-rays can provide limited information about the heart’s condition. Chest X-rays are used to provide the doctor with a view of both the heart and lungs to help determine if any abnormalities are present. These two X-rays show a relatively normal heart on the left. In the right X-ray, an enlarged heart (mainly the left ventricle) is easily seen and suggests the heart's main pumping chamber is not functioning normally. In addition, x-rays may show fluid accumulation in the lungs, possibly from heart failure.
17 of 29
Heart Disease Testing: Echocardiogram
An echocardiogram is a real-time moving picture of a functioning heart made by using sound waves (ultrasound) to generate images. Echocardiograms use the same noninvasive technology used to examine the fetus during pregnancy. It can show how well heart chambers and heart valves are functioning (for example, effective or poor pumping action, blood flow through the valves), before and after treatments, as well as other features.
18 of 29
Heart Disease Testing: Cardiac CT Scan
Specialized cardiac computerized tomography (CT) scans or ‘cardiac CTs’ can provide detailed 3-D images of the heart. The images can be manipulated to look for calcium buildup (plaque) in coronary arteries or provide images of such internal structures of the heart like valves or wall thickness. CTs can also be used to examine normal heart anatomy or congenital defects. The information from a CT can provide insight into several heart disease problems.
19 of 29
Heart Disease Testing: Cardiac Catheterization
Plaque in cardiac arteries can be a severe problem, even life-threatening, in some patients. Diagnosing plaque blockage of coronary arteries and treatment for blockages has improved the lives of many patients with coronary artery disease. Cardiac catheterization is a technique that may provide both diagnostic information and therapeutic methodology in one procedure. The technique is invasive.
How Cardiac Catheterization Works
A thin tube is placed in a blood vessel in the leg or arm and threaded into the heart and into the opening of a coronary artery.
Dye is put into the tube and goes into the artery.
A special X-ray machine images the dye, showing narrowing or blockage of the artery.
The same tube may be used with special tips to open the coronary artery by angioplasty (small balloon is inflated) or used to place a wire mesh (stent) that expands to hold the artery open.
20 of 29
Living With Heart Disease
Most types of heart disease are chronic but slowly progressive like heart failure or cardiomyopathy. They begin with minor symptoms that often slowly worsen and require long-term medical treatment.
Symptoms That May Resist Treatment
Ankle swelling
Fatigue
Fluid retention
Shortness of breath
Lifestyle changes may become necessary (for example, home oxygen, limited activity
21 of 29
Heart Disease Treatment: Medicines
Advances in medicines that can help reduce the symptoms and slow the damage of heart disease have helped the majority of heart disease patients. Drugs are available to do the following:
Lower blood pressure (anti-hypertensives)
Lower heartbeat rates (beta blockers)
Lower cholesterol levels to reduce plaque (diet, statins)
Help stabilize abnormal heart rhythms (ablation, cardiac pacers)
Reduce or prevent clotting in coronary arteries (blood thinners)
Improve the pumping ability of a person's heart with heart disease (inotropic agents)
22 of 29
Heart Disease Treatment: Angioplasty
Other treatments for heart disease involve special techniques like angioplasty and stent placement.
Angioplasty Step by Step
A thin catheter or tube (stent) is placed in a coronary artery and is threaded through an obstruction like a clot.
A balloon is inflated and pushes aside the obstruction.
The balloon is then deflated leaving the artery unblocked, thus allowing good blood flow.
Often, after angioplasty, an expandable mesh tube is then inserted and expanded, reinforcing the artery to keep it from collapsing.
23 of 29
Heart Disease Treatment: Bypass Surgery
Some patient's coronary arteries are not good candidates for angioplasty and/or stents. Such patients may benefit from another treatment technique termed bypass surgery. Bypass surgery occurs when a surgeon removes a blood vessel from one part of the body (chest, legs, or arms) and uses it to connect one open part of a coronary artery to another open part, thus bypassing the area that has blocked blood flow. Often the surgeon may need to bypass more than one artery.
The decision to try and stent a coronary artery versus doing bypass surgery is usually recommended to the patient by their cardiologist and a heart surgeon. Bypass surgery is usually done if coronary arteries are narrowed or blocked in multiple places.
24 of 29
Who Is at Risk for Heart Disease?
Health conditions, lifestyle, age, and family history may increase your risk for heart disease. Although men, even at a younger age, have a higher risk for heart disease than women, heart disease is still the number one killer of both sexes (about 611,000 total deaths/year). People with a family history of heart disease, who smoke, and who are obese have a higher risk of developing heart disease. About half of all Americans (47%) have at least one of three key risk factor for heart disease including high blood pressure, high cholesterol, or smoking.
25 of 29
Controllable Heart Disease Risks
Often, risk factors for heart disease can be managed or reduced through simple methods. Common risk factors for heart disease include the following:
Heart Diseases Risks You Can Control
Diabetes
Elevated cholesterol
High blood pressure
Lack of physical activity
Stop smoking
These risk factors can be reduced simply by making healthy lifestyle choices and taking medications. Your primary care doctor can help you with your choices and medications.
26 of 29
Smoking Increases Heart Disease Risk
Many researchers suggest one of the best things a person can do to decrease the risk of heart disease is to stop smoking cigarettes. Smoking increases a person's risk for heart disease from 2 to about 4 times greater than nonsmokers. Smoking can damage the heart muscle, its blood vessels, can raise blood pressure, increase carbon monoxide levels, and reduce oxygen available to heart tissue.
People who do not smoke but are exposed to second-hand smoke are at greater risk for heart disease than those not exposed to second-hand smoke. Although over 135,000 people die each year from heart disease related to smoking, it is never too late to quit smoking because once you quit, your risk of heart disease begins to drop almost immediately.
27 of 29
Life After a Heart Attack
Don’t give up activities if you have a heart attack. If a person suffers a heart attack, it is still possible to develop a healthy lifestyle. Many doctors recommend that their patients participate in a cardiac rehab program and learn how to avoid cigarettes, develop a healthy diet, and become more active. All of these changes may help a person’s heart recover and function better and to reduce the chance of additional heart problems.
28 of 29
Preventing Heart Disease
Heart disease prevention and risk reduction is possible by living a healthy lifestyle. Basic components of a heart-healthy lifestyle include:
Never smoke or stop smoking cigarettes (and using other tobacco products)
Eat a nutritious diet (many vegetables and fruits, less fats, sugars, and meats)
Get at least 30 minutes of exercise almost every day
Avoid alcohol or consume no more than 1 drink per day for women and no more than 2 drinks per day for men
If needed, achieve medical control of diabetes, high blood pressure, and cholesterol
Encourage friends and family to help you. Maybe they could benefit from your good example!
29 of 29
Heart Disease and Diet
A major key to preventing, recovering from, and slowing heart disease is a heart-healthy diet. Most heart doctors recommend the following foods.
Heart-Healthy Foods
Fruits
Legumes
Vegetables
Whole grains
Foods That May Help Reduce Cholesterol Levels
Nuts
Plant oils
Seeds
Eating fish about twice a week is a good source of protein without the fats found in red meat. Some researchers have suggested that a more vegetarian-like diet may actually reverse some aspects of coronary artery disease like plaque size.
While heart disease is treatable by many methods, prevention or healing by living a reasonable lifestyle seems to be one of the best ways to reduce this widespread health problem
Stay safe , stay healthy
from this site found it interesting from this site found it interesting https://www.medicinenet.com/script/main/mobileart.asp?articlekey=120006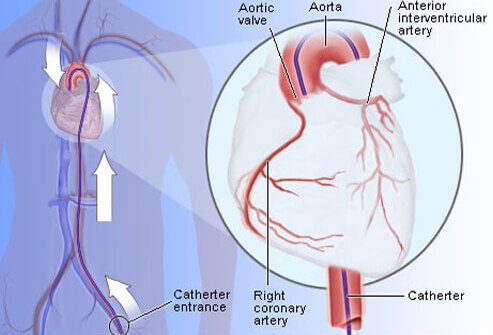
Hi! I am a robot. I just upvoted you! I found similar content that readers might be interested in:
https://www.onhealth.com/content/1/heart_disease